100Views 0Comments
When most people think of physiotherapy, they often picture athletes recovering from injuries. However, physiotherapists play a crucial role in intensive care units (ICUs) as well.
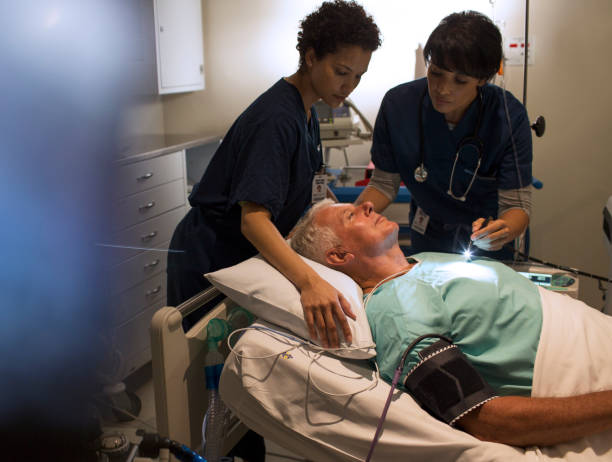
ICUs are often the last resort for patients with life-threatening illnesses or injuries. Patients in the ICU are usually connected to various types of life support equipment, such as ventilators, and are closely monitored by a team of healthcare professionals.
Intensive Care Units (ICUs) are specialized wards in hospitals where critically ill patients receive life-saving care. Patients in the ICU often require complex interventions, including mechanical ventilation, dialysis, and vasoactive medications. The goal of care in the ICU is to stabilize the patient’s condition and prevent complications. One important aspect of ICU care is physiotherapy. In this article, we will discuss the role of physiotherapy in the ICU, and its effectiveness in improving patient outcomes.
Physiotherapy in the ICU
Physiotherapy is an important component of ICU care. Physiotherapists work closely with other members of the healthcare team to optimize patients’ physical function and mobility, prevent complications, and improve overall patient outcomes. Physiotherapists in the ICU provide a range of interventions, including early mobilization, breathing exercises, and airway clearance techniques.
Early Mobilization
Early mobilization is a key component of physiotherapy in the ICU. It involves getting patients up and moving as soon as possible after they are admitted to the ICU. Early mobilization has been shown to improve muscle strength, physical function, and reduce the duration of mechanical ventilation in critically ill patients. Early mobilization has also been associated with a reduced risk of delirium, which is a common complication in critically ill patients. The following are the early mobilization techniques:
- Bed Mobility
The first step in early mobilization is bed mobility. Bed mobility exercises involve helping patients change positions in bed. These exercises can include turning from side to side, sitting up in bed, and standing up with assistance. Bed mobility exercises are important for preventing pressure sores, improving respiratory function, and maintaining range of motion.
- Sitting on the Edge of the Bed
The next step in early mobilization is sitting on the edge of the bed. Sitting on the edge of the bed helps to improve balance and coordination and prepares patients for standing and walking. Patients should be assisted to sit up with their legs over the edge of the bed and their feet on the ground. This exercise can be performed multiple times per day.
- Standing
Standing is an important part of early mobilization in the ICU. Standing helps to improve muscle strength, cardiovascular function, and respiratory function. Patients should be assisted to stand up with support, such as a standing frame or a walker. The duration of standing can be gradually increased as the patient’s strength and endurance improve.
- Walking
Walking is the final step in early mobilization in the ICU. Walking helps to improve cardiovascular function, muscle strength, and endurance. Patients should be assisted to walk with support, such as a walker or a gait belt. The duration and distance of walking can be gradually increased as the patient’s strength and endurance improve.
- Range of Motion Exercises
Range of motion exercises are an important part of early mobilization in the ICU. Range of motion exercises help to maintain joint flexibility and prevent contractures. Range of motion exercises can include gentle stretching and bending of the joints.
6. Other Techniques
Other techniques used in early mobilization in the ICU can include passive range of motion exercises, resistance training, and balance training. Passive range of motion exercises involve moving the patient’s joints through their full range of motion without any effort from the patient. Resistance training involves using weights or resistance bands to improve muscle strength. Balance training involves exercises to improve balance and coordination.
Breathing Exercises

Breathing exercises are another important component of physiotherapy in the ICU. These exercises are designed to improve lung function and prevent complications such as pneumonia. Breathing exercises can include deep breathing, coughing, and incentive spirometry. These exercises help to promote airway clearance, increase lung volumes, and improve gas exchange in critically ill patients.
In this article, we will discuss some of the techniques used for breathing exercises in the ICU.
- Deep Breathing
Deep breathing exercises are a simple and effective technique for improving lung function in the ICU. This technique involves taking slow, deep breaths in through the nose and out through the mouth. Patients can perform this exercise while lying in bed or sitting up.
- Coughing
Coughing is another important technique for improving lung function in the ICU. Coughing helps to clear mucus from the airways and prevent pneumonia. Patients should be encouraged to cough deeply and effectively. If necessary, a physiotherapist can provide assistance with techniques such as splinting the chest wall or suctioning.
- Incentive Spirometry
Incentive spirometry is a technique that involves using a device to help patients take deep breaths and improve lung function. The device consists of a plastic tube with a mouthpiece attached to one end and a chamber with a piston inside. Patients inhale through the mouthpiece and try to lift the piston as high as possible by taking deep breaths. This technique can be used several times a day to improve lung function.
- Positive Expiratory Pressure (PEP) Therapy
Positive expiratory pressure (PEP) therapy is a technique that involves using a device to help patients breathe out against resistance. The device consists of a mouthpiece attached to a valve that creates resistance during exhalation. This technique helps to improve lung function by keeping the airways open and clearing mucus from the lungs.
- High-Frequency Chest Wall Oscillation (HFCWO)
High-frequency chest wall oscillation (HFCWO) is a technique that involves using a device to vibrate the chest wall and help loosen mucus in the lungs. The device consists of an inflatable vest that is worn around the chest. The vest inflates and deflates rapidly, creating vibrations that help to loosen mucus in the lungs. This technique can be used several times a day to improve lung function.
- Diaphragmatic Breathing
Diaphragmatic breathing is a technique that involves using the diaphragm muscle to improve lung function. The diaphragm is a large muscle located below the lungs that helps to control breathing. Patients can practice diaphragmatic breathing by lying on their back with a pillow under their knees, placing one hand on their chest and the other hand on their abdomen, and breathing in deeply through their nose and out through their mouth while focusing on the movement of their abdomen.
Airway Clearance Techniques

Airway clearance techniques are used to help clear secretions from the lungs and airways in critically ill patients. These techniques can include chest physiotherapy, vibration, and postural drainage. These interventions help to prevent complications such as pneumonia, and improve overall respiratory function in critically ill patients. Now
we will discuss some of the airway clearance techniques used in the ICU.
- Chest Physiotherapy (CPT)
Chest physiotherapy (CPT) is a manual airway clearance technique used to help patients with respiratory conditions to clear secretions from their lungs. Chest physiotherapy (CPT) is a technique that involves using various manual techniques to help clear secretions from the lungs. These techniques include percussion, vibration, and postural drainage.
The percussion technique involves the use of a cupped hand or a mechanical device to gently tap on the chest wall and back of the patient. This tapping helps to create vibrations that loosen secretions and help to move them up towards the larger airways, where they can be coughed up more easily.
The vibration technique involves the use of a mechanical device that delivers high-frequency vibrations to the chest wall and back of the patient. These vibrations help to loosen secretions and move them up towards the larger airways.
Postural drainage involves positioning the patient in various positions to allow gravity to help move secretions towards the larger airways. For example, a patient with secretions in the lower lobes of the lungs may be positioned with their feet elevated to allow the secretions to move towards the upper lobes of the lungs, where they can be coughed up more easily.
CPT is often used in patients who are unable to cough effectively or who have thick or sticky secretions. It can be performed by a physiotherapist or a respiratory therapist, and can be done manually or with the use of mechanical devices.
It is important to note that CPT should only be performed by a trained healthcare professional, as incorrect technique can lead to injury or discomfort for the patient. Patients should also be closely monitored during CPT to ensure that it is being performed safely and effectively.
CPT is often used in conjunction with other airway clearance techniques to improve lung function, prevent complications such as pneumonia, and improve overall patient outcomes. A physiotherapist will assess the patient and develop a treatment plan that is tailored to their specific needs.
- High-Frequency Chest Wall Oscillation (HFCWO)
High-frequency chest wall oscillation (HFCWO) is a technique that involves using a device to vibrate the chest wall and help loosen mucus in the lungs. The device consists of an inflatable vest that is worn around the chest. The vest inflates and deflates rapidly, creating vibrations that help to loosen mucus in the lungs.
- Positive Expiratory Pressure (PEP) Therapy
Positive expiratory pressure (PEP) therapy is a technique that involves using a device to help patients breathe out against resistance. The device consists of a mouthpiece attached to a valve that creates resistance during exhalation. This technique helps to improve lung function by keeping the airways open and clearing mucus from the lungs.
- Oscillating Positive Expiratory Pressure (OPEP) Therapy
Oscillating positive expiratory pressure (OPEP) therapy is a technique that combines positive expiratory pressure (PEP) therapy with oscillations. The device consists of a mouthpiece and a valve that creates resistance during exhalation, as well as a vibrating mechanism that creates oscillations. This technique helps to loosen mucus in the lungs and improve lung function.
- Nebulized Bronchodilator Therapy
Nebulized bronchodilator therapy is a technique that involves using a nebulizer to deliver medication directly to the lungs. The medication helps to open up the airways and improve lung function. This technique is often used in conjunction with other airway clearance techniques.
6. Active Cycle Of Breathing Technique(ACBT)
Active Cycle of Breathing Technique, which is a breathing technique used by physiotherapists to help patients with respiratory conditions to clear secretions from their lungs. It involves three phases: breathing control, thoracic expansion exercises, and forced expiratory techniques.
Breathing Control Phase:
The first phase of ACBT is breathing control. This phase involves controlled breathing exercises, such as diaphragmatic breathing, to help patients achieve a state of relaxation and to control their breathing. This helps to reduce the work of breathing and conserve energy, which is important for patients who are already struggling to breathe.
Thoracic Expansion Exercises Phase:
The second phase of ACBT is thoracic expansion exercises. This phase involves deep breathing exercises to help expand the chest and mobilize secretions. The patient takes a deep breath, holds it for a few seconds, and then slowly exhales while hunching forward. This technique helps to expand the chest and mobilize secretions, making them easier to clear from the lungs.
Forced Expiratory Techniques Phase:
The third phase of ACBT is forced expiratory techniques. This phase involves coughing and huffing to help clear secretions from the lungs. The patient takes a deep breath and then coughs or huffs forcefully to clear secretions from the lungs. This technique helps to move secretions up from the small airways in the lungs to the larger airways, where they can be coughed up more easily.
ACBT is a safe and effective technique for patients with respiratory conditions. It can be used in a variety of settings, including in the hospital, in the home, and in outpatient clinics. Patients should be closely monitored by a physiotherapist to ensure that the technique is performed safely and effectively. ACBT is often used in conjunction with other airway clearance techniques to improve lung function, prevent complications such as pneumonia, and improve overall patient outcomes.
Effectiveness of Physiotherapy in the ICU

Physiotherapy is an important component of ICU care, but what is the evidence to support its effectiveness? A number of studies have been conducted to evaluate the effectiveness of physiotherapy in the ICU, and the results are promising.
One study conducted by Schweickert et al. (2009) found that early mobilization in the ICU was associated with a significant reduction in the duration of mechanical ventilation and ICU length of stay. Patients who received early mobilization also had improved physical function at hospital discharge.
Another study conducted by Morris et al. (2016) found that physiotherapy interventions, including early mobilization, breathing exercises, and airway clearance techniques, were associated with a significant reduction in the risk of delirium in critically ill patients. Delirium is a common complication in the ICU and is associated with increased morbidity and mortality.
A systematic review conducted by Tipping et al. (2015) found that early mobilization in the ICU was associated with a significant reduction in the incidence of ventilator-associated pneumonia, and a significant improvement in physical function.
conclusion
Physiotherapy is an important component of ICU care, and the evidence supports its effectiveness in improving patient outcomes. Physiotherapists in the ICU provide a range of interventions, including early mobilization, breathing exercises, and airway clearance techniques, to optimize patients’ physical function and mobility, prevent complications, and improve overall patient outcomes.
Future research in this area should focus on identifying the most effective physiotherapy interventions for critically ill patients, and determining the optimal timing and duration of these interventions. With continued research and innovation, physiotherapy will remain a vital component of ICU care, improving


