158Views 0Comments

One of the most intricate joints in the human body, the shoulder joint allows for a large range of motion and flexibility.
A healthcare provider would often start a shoulder joint examination by questioning the patient about any symptoms they may be having, such as pain, stiffness, or weakness in the shoulder. They could also inquire about any past illnesses or injuries that might have contributed to the symptoms.
The healthcare expert will then examine the shoulder joint physically. This may entail evaluating the shoulder muscles’ strength, the joint’s range of motion, and any indications of swelling or inflammation.
X-rays, MRIs, or ultrasound imaging may be requested in addition to the physical examination depending on the results in order to obtain a more thorough image of the shoulder joint.
In order to rule out any underlying diseases or injuries that might be causing shoulder pain or other symptoms, it’s critical to do an assessment. With this knowledge, medical experts may create a treatment plan that will meet the patient’s unique needs and promote a speedy and safe recovery.
physiotherapy assessment
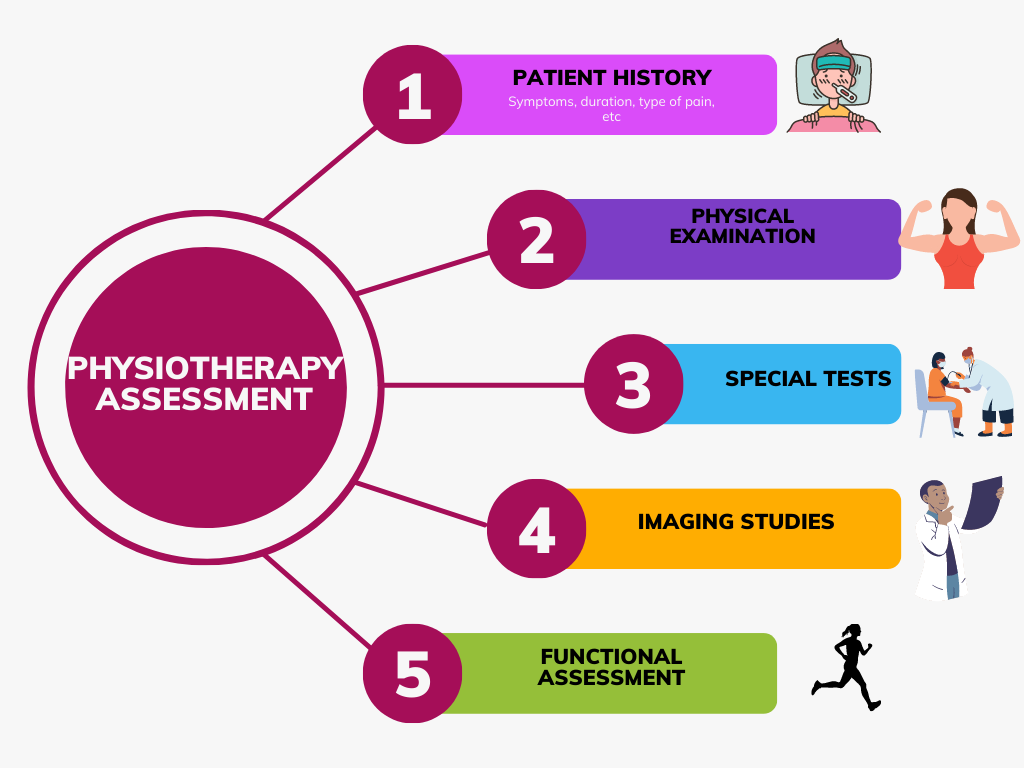
A complete assessment of the patient’s shoulder function and range of motion is usually part of a physiotherapy assessment of the shoulder joint. A certified physiotherapist typically conducts the evaluation, which could include the following elements:
Patient history: The physiotherapist will inquire about the patient’s symptoms, medical background, and any prior shoulder joint issues.
Physical examination: The physiotherapist will carry out a physical assessment of the shoulder joint. This examination will include exercises to measure the strength, flexibility, and range of motion of the muscles and joints in the shoulder and its surrounding region.
Special tests:Tests specifically designed to evaluate the stability of the shoulder joint include the anterior drawer test, the apprehension test, and the sulcus sign.
Imaging studies: To obtain a more thorough image of the shoulder joint, the physiotherapist may request imaging tests like X-rays, MRI scans, or ultrasound imaging, depending on the findings of the physical examination.
Functional assessment: The physiotherapist may evaluate the patient’s capacity to carry out functional tasks, such as reaching up or lifting objects, and activities of daily living.
The physiotherapist will create a treatment plan unique to the patient’s requirements based on the findings of the examination. Exercises to increase range of motion, strength, and flexibility may be part of the course of treatment, along with manual therapy, modalities like ultrasound or electrical stimulation, and instruction on good posture and body mechanics to prevent further injury.
Patient history
The patient’s history is a crucial part of the evaluation when a patient is evaluated for an issue involving the shoulder joint. A thorough patient history can assist the healthcare professional in identifying the underlying cause of the patient’s symptoms and determining the best course of action. During a patient history evaluation for the shoulder joint, healthcare professionals could inquire about the following details:
Symptoms: The doctor will inquire about the patient’s symptoms, such as pain, stiffness, weakness, instability, and popping or clicking noises.
Prior injuries or operations: The medical professional will enquire about any prior injuries or operations the patient may have had on the shoulder joint.
Medical history: The doctor will enquire about the patient’s medical background, particularly any chronic illnesses like diabetes or arthritis.
Family history: The medical professional may inquire about the patient’s family history of joint issues or other illnesses.
Lifestyle and activities: To identify any probable reasons of the shoulder joint issues, the healthcare professional may inquire about the patient’s job, interests, and athletic activities.
Medication: The healthcare professional will inquire about any prescription, over-the-counter, and herbal supplements the patient is currently using.
Allergies: The medical professional will enquire about the patient’s allergies, including those to drugs or other substances.
Physical examination
A set of tests and assessments are commonly used during a physical examination of the shoulder joint to gauge its stability, strength, and range of motion. A healthcare professional may do the following physical examination tests while evaluating the shoulder joint:
The healthcare professional may watch the patient’s posture, how they stand, and any muscular atrophy or asymmetry.
Range of motion: To measure the patient’s range of motion, the healthcare professional may ask them to move their arm in various directions. This may entail abduction, internal and external rotation, horizontal adduction, and abduction, as well as forward flexion.
Muscular strength: By asking the patient to exert resistance against it, the healthcare professional can determine how strong the patient’s shoulder muscles are.
Joint stability: The healthcare professional may undertake specific tests, such as the apprehension test, the anterior drawer test, or the sulcus sign, to determine the stability of the shoulder joint.
Palpation: The medical professional may use their hands to feel the shoulder joint and the surrounding area for any soreness, edema, or abnormalities.
Neurovascular assessment: In order to rule out any nerve or blood vessel problems, the healthcare professional may examine the patient’s sensation and circulation in the arm and shoulder.
Special tests: Tests specifically designed to evaluate the patient’s rotator cuff, labrum, biceps, and other shoulder joint structures may be carried out by the medical professional.
special tests

A complicated joint, the shoulder’s range of motion is extensive. In order to evaluate the stability of the shoulder joint and surrounding structures, a number of specialized tests may be utilized. These examinations can aid in locating specific shoulder problems or ailments. Some of the most popular special tests for the shoulder joint are listed below:
Neer’s Test: This test is performed to determine whether the rotator cuff tendons are impinged. When lifting the arm, the examiner internally rotates the patient’s shoulder. If there is impingement, this squeezes the rotator cuff tendons up against the acromion process and causes pain.
Hawkins-kennedy test: The Hawkins-Kennedy test is also used to determine whether the rotator cuff is impinged.The examiner forces the arm to be internally rotated after flexing the patient’s shoulder to 90 degrees. The rotator cuff tendons are impinged upon when performing this motion, which causes pain.
Speed test: The Speed’s Test is used to evaluate the health of the biceps tendon. As he or she is resisting, the examiner urges the patient to flex their arm. Biceps tendonitis or a potential SLAP injury are both indicated by pain in the bicipital groove.
Yergason’s Test: This test is also used to detect pathology in the biceps tendon. As he or she is resisting, the examiner urges the patient to supinate their forearm. Biceps tendonitis or a potential SLAP injury are both indicated by pain in the bicipital groove.
Empty can test: The empty can test is performed to determine whether the supraspinatus muscle is weak or torn. In the “empty can posture,” the examiner raises the patient’s arm to 90 degrees in the scapular plane while resisting abduction. A supraspinatus tear or impingement is indicated by pain or weakness during this movement.
Drop arm test: The Drop Arm Test is performed to determine whether the supraspinatus muscle is weak or torn. The patient is asked to slowly lower their arm to their side after the examiner passively raises their arm to 90 degrees. A supraspinatus tear is present if the patient is unable to regulate the descent of their arm.
Test of Apprehension: This test evaluates shoulder instability. The examiner externally rotates the patient’s shoulder while abducting the patient’s arm to 90 degrees. When performing this maneuver, discomfort or anxiety implies anterior shoulder instability.
Relocation test: This test is also utilized to evaluate shoulder instability. The patient is in the apprehension posture and the examiner administers a posteriorly directed force to the anterior shoulder. This maneuver’s capacity to relieve pain points to anterior shoulder instability.
Sulcus Sign: This test determines whether the inferior shoulder is unstable. The examiner drags the patient’s arm downward while looking for an indentation (sulcus) at the shoulder joint. A sulcus shows instability in the inferior shoulder.
imaging studies
The shoulder joint can be examined using a variety of imaging procedures. A sort of imaging examination called an arthrography is used to examine a joint, such as the shoulder, knee, or hip, according to Johns Hopkins Medicine. If common X-rays fail to provide the necessary information on the structure and function of the joint, it might be done. A series of X-rays are taken with the joint in various positions during arthrography, which involves inserting contrast dye directly into the joint with a long, thin needle.
Plain radiography (X-rays), ultrasonography, computed tomography (CT), and MRI scans are further imaging possibilities for shoulder issues. CT can show fracture complexity, displacement, and angulation, and is typically used to evaluate fracture/fracture-dislocation or a prosthetic joint. MRI scans, on the other hand, make use of sound waves to create images of the body’s structures, particularly soft tissues like muscles and tendons, enabling a fast comparison of the injured shoulder and the healthy shoulder.
functional assessment
The functional assessment of the shoulder joint is a crucial step in the evaluation process because it can reveal the degree of the patient’s impairments, activity constraints, and participation restrictions. The following functional tests for the shoulder joint are frequently used:
Constant-Murley Score: This is a subjective and objective scoring system that evaluates discomfort, functional limitations associated with daily life, range of motion, and shoulder joint strength. It is frequently employed to assess people who have rotator cuff problems.
QuickDASH: Using the afflicted shoulder joint, this questionnaire assesses the patient’s capacity to carry out daily tasks. It has 11 items that evaluate various actions including opening doors, reaching up, and carrying things.
Simple Shoulder Test (SST): This is a questionnaire that assesses the patient’s capacity to use the injured shoulder joint for daily activities. It comprises of 12 items that evaluate various tasks like lifting, reaching, and sleeping.
Shoulder Pain and Disability Index (SPADI): The Shoulder Pain and Disability Index (SPADI) is a questionnaire used to assess a patient’s level of pain and functional impairment as a result of shoulder joint issues. It comprises of 13 items that evaluate various facets of discomfort and incapacity.
Upper Extremity Functional Index (UEFI): The patient’s capacity to use the affected upper extremity, which includes the shoulder joint, for daily activities is assessed using the Upper Extremity Functional Index (UEFI), a questionnaire. It comprises of 20 items that evaluate various actions like lifting, transporting, and getting dressed.
Functional evaluations can offer important details on the patient’s physical limitations, level of pain, and capacity for everyday activities. They can also be used to measure how well therapy strategies are working and to track development over time.